Collagen crosslinking uses ultraviolet (UV) light combined with riboflavin (Vitamin B2). The primary goal of collagen crosslinking in the keratoconic patient is to strengthen and stiffen the corneal fibers in order to decrease the progression of keratoconus, and to decrease the cone steepness in some patients.
The Crosslinking Procedure
CXL is performed at the state of the art Kornmehl Laser Eye Associates by Dr. Ernest W. Kornmehl. Anesthesia eye drops keep you comfortable and a lid speculum prevents you from blinking. The surface epithelial cells of the cornea are removed and then riboflavin drops are administered for 30 minutes. The riboflavin acts both to enhance the crosslinking effect and to protect the rest of the eye from the UV exposure.
The patient then looks at a UV emitting light (wavelength= 365 microns, power= 3.0 mW/cm2) for 30 additional minutes with continued administration of riboflavin drops. At the conclusion of the procedure, a soft bandage contact lens is applied. The contact lens is left in place to improve healing for approximately 5 days and is then removed. Antibiotic and anti-inflammatory drops are used for at least two weeks afterwards.
If you have an interest or have any questions about collagen crosslinking, please call our office or email us at info@visionboston.com
What is Keratoconus?
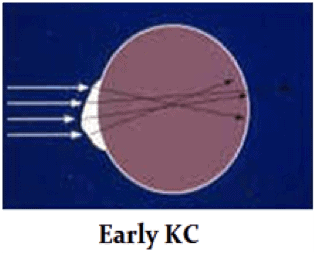
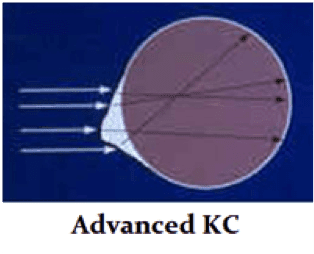
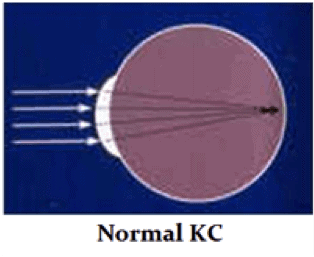 Keratoconus, one of the more obscure and less widely known eye diseases, occurs in about one out of every 1,000 individuals. It is also one of the more difficult eye diseases to diagnose. The disease results in thinning and weakening of the cornea, the clear lens that is the front of the eye (like the crystal on a watch). As a result, the cornea bulges out of its smooth, dome-like structure, and assumes a more conical and irregular configuration. Due to this change in shape, the cornea loses its ability to form a clear image in the eye and the patient’s vision can decrease drastically. Why is this? Optically, in the keratoconic cornea, light is not completely focused because of the corneal distortion. This causes scattering of light rays and the formation of “visual static”, much like the static that you may find on a TV. This distortion, and consequent visual static, can increase over time, with decrease in vision.
Keratoconus, one of the more obscure and less widely known eye diseases, occurs in about one out of every 1,000 individuals. It is also one of the more difficult eye diseases to diagnose. The disease results in thinning and weakening of the cornea, the clear lens that is the front of the eye (like the crystal on a watch). As a result, the cornea bulges out of its smooth, dome-like structure, and assumes a more conical and irregular configuration. Due to this change in shape, the cornea loses its ability to form a clear image in the eye and the patient’s vision can decrease drastically. Why is this? Optically, in the keratoconic cornea, light is not completely focused because of the corneal distortion. This causes scattering of light rays and the formation of “visual static”, much like the static that you may find on a TV. This distortion, and consequent visual static, can increase over time, with decrease in vision.
Biologically and structurally, the cornea is made up of pancakes (lamellae) of collagen protein which are “glued” together by natural biologic sugars (called glycosaminoglycans or GAG’s). Both the collagen and microstructure of the cornea are abnormal in keratoconus, causing a weakness of the corneal structure which then leads to optical problems. It is a progressive condition which, aside from distorting the cornea’s natural optics, can also lead to scarring and other problems.
The presentation and impact of keratoconus can widely vary from person to person. In its earliest stages, keratoconus often masquerades as astigmatism or nearsightedness, two of the more common eye conditions. Corneal topographic mapping is used to verify this diagnosis which is not typically performed during a routine eye exam. It is imperative to schedule a consultation with Dr. Kornmehl if you have encountered numerous unsuccessful attempts at vision correction with glasses or contact lenses.
What Causes Keratoconus?
The actual cause of keratoconus is unclear. It may have a genetic, inheritable component. However, in many patients there is no family history with the disease. Similarly, most children of KC patients do not have keratoconus, but they should be checked in early adolescence for signs of KC.
Keratoconus is typified by corneal thinning and biomechanical instability. This may be caused by abnormalities in the normal collagen structure of the cornea. Collagen is the main structural component of the cornea. Collagen is a molecule that typically is very strong. For example, it makes up most of the structure of the tendons and ligaments of your muscles and bones. The cornea is made of pancakes of collagen tissue in a complex array. In keratoconus, the collagen lamellar architecture may be abnormal. There may also be abnormal enzymes which degrade the collagen and reduce the amount of collagen in the KC cornea.
In addition, the cells of the cornea (keratocytes), may not be normal, and contribute to the thinning and instability of the keratoconic cornea.
The linkages of the collagen molecules and lamellae to one another may also be weak in keratoconus. For instance, “anchoring fibrils” which normally lock the collagen pancakes to the front of the cornea, on Bowman’s layer, may be abnormal. This may allow the collagen pancakes to slide on one another and exacerbate KC progression. It is vital that the keratoconus patient does not rub his/her eyes in order to avoid mechanical shearing of the collagen pancakes.
Finally, inflammation may also play a role in keratoconus. Reactive oxygen species, or oxygen free radicals, may damage the corneal cells and collagen structure, and lead to keratoconus progression. Avoiding and treating eye inflammation (for instance, eye allergies) is extremely important for the patient with KC.
At Kornmehl Laser Eye Associates, we are working to identify factors that might place the keratoconus patient at greater risk, while we bring our patients the best treatment options available.
Collagen Cross-linking Frequently Asked Questions
What is the safety profile regarding the use of ultra-violet light and of riboflavin in the eye?
The ultraviolet light exposure during the cross-linking procedure is comparable to, or even less than, the exposure of the eye to the ultraviolet light in skylight for a full day outdoors in the summer. The riboflavin drops are simply vitamin B2, commonly used in foods such as your breakfast cereal.
How many people have undergone a cross-linking procedure?
Thousands of people have had their corneas cross-linked in Europe during the past 13 years. Due to the universal acceptance of the benefits of cross-linking among ophthalmologists, and recent advances in technology, the annual number of cross-linking procedure is expected to increase substantially.
What are the possible complications and side effects of cross-linking?
Discomfort in the first 1-2 days, sensitivity to light for several days, haze within the cornea that may cause blurring for up to a few weeks. There are other, more severe and less common, possible side effects. For a more comprehensive list of possible side effects, please see the details of the informed consent.
Am I asleep for the treatment?
No. You will be awake for the treatment. You will be given relaxing medication and anesthetic drops to numb any sensation or discomfort.
Does it hurt?
There is some discomfort during immediate recovery but not during the treatment. Immediately following treatment, a bandage contact lens is placed on the surface of the eye to protect the newly treated area. After the numbing drops wear off, there is some discomfort, often described as a gritty, burning sensation. These are managed with punctum plugs, medicated antibiotic and anti-inflammatory eye drops along with artificial tears and percocet.
How long does the treatment take?
Actual treatment for each eye takes about 1 hour, but you will be at the office for roughly 2 hours to allow sufficient time for preparation and recovery before you return to the comfort of your own home.
What results can I expect?
Individual results vary but most people’s vision returns to pre-operative status and return to driving and work within 1 week. Some degree of cloudiness/ blurriness is expected to last up to 1 month. Although this procedure is specifically intended to halt the progression of thinning, your astigmatism may reduce as recovery progresses, usually over a 6-12 month period after treatment.
Can cross-linking be redone if needed?
Yes, but during the past 13 years a one-time treatment has been shown generally to be enough to treat progression.
Can both eyes be cross-linked at the same time?
Technically yes, but most patients have one eye done at a time.
Will this be covered under insurance in the future?
We believe this is the next phase in cornea care for patients with keratoconus or post- refractive ectasia. In the future, we anticipate coverage by insurance companies. At this point, it is not being covered by insurance.
Will I need to be out of my contact lenses for this process?
Yes, Contact lenses can warp the cornea. It is the goal of cross-linking to strengthen the cornea in its natural state. In order to allow for contact lens induced warpage to reduce, patients must discontinue the use of contact lenses before the screening. Many times, this will require additional visits to achieve stability. Once treated, patients will not be allowed back into contact lenses for 1 month.